
Fighting Inflammation with Food
Early this week, The Whole U partnered with UW Medical Center Registered Dietitian, Charlotte Furman, to offer a seminar discussing the current research on inflammation – including associated diseases, the role of the gut microbiome, and the influence of our food choices.
As the new nutrition intern for the Whole U (and a public health nutrition graduate student here at UW), I was very excited to be among experts in the field and increase awareness surrounding the importance of food and diet in disease prevention and overall wellness. In case you weren’t able to attend the seminar, I’ve put together a brief recap so you can see why you should combat the negative effects of inflammation – and how.
What is Inflammation?
Inflammation is our body’s normal immune response to injury or harm, like the redness and swelling you might see when you get a cut on your finger. This type of acute (short-term) inflammation serves as a protective mechanism by releasing several pro-inflammatory cytokines.
However, chronic (long-term) inflammation can actually cause tissue damage and contribute to certain diseases, including:
- diabetes
- arthritis
- heart disease
- cancer
- depression
- Alzheimer’s
(You can learn more about inflammation’s role in these diseases here, here, and here)
Getting a Good Gut Microbiome
Certain foods and food patterns can be pro- or anti-inflammatory. A pro-inflammatory diet consists of:
- refined carbohydrates (white bread)
- refined vegetable oils (corn, soy, sunflower, and safflower—found in fried foods)
- sugar-sweetened beverages (soda)
- red and processed meats
- trans fats (partially hydrogenated oils)
This type of diet includes many components of a typical American diet and can lead to a less diverse gut microbiome, meaning less friendly bacteria. Including pre- and probiotics in your diet can improve the gut’s immune function and inhibit inflammatory processes that can damage your gut cells. Research has shown that diet modifications can result in changes in gut microbiota in a matter of four weeks.
Prebiotics are indigestible plant fibers that provide nourishment to beneficial bacteria and can be found in onions, garlic, fruits (bananas), vegetables (asparagus, artichoke), and whole grains.
Probiotics are live microorganisms that benefit the host, and can be found in fermented foods such as yogurt, kefir, kimchi, miso, tempeh, sauerkraut, and kombucha.
The Omega Problem
Another important component of an anti-inflammatory diet is keeping an omega-6 to omega-3 intake ratio of about 4:1. The current ratio of the average American diet is estimated to be at 20:1, much higher than ideal. Omega-6 fatty acids metabolize into pro-inflammatory compounds, whereas omega-3 fatty acids metabolize into more favorable compounds.
Omega-6 fatty acids (arachidonic acid) can be found in corn-fed animal products, and oils such as corn, sunflower, soy, and cottonseed.
Omega-3 fatty acids (EPA and DHA) can be found in fish, walnuts, dark leafy greens, grass-fed animal products, and oils such as flax, canola, and camelina.
Anti-Inflammatory Diets
Various studies have provided evidence for the anti-inflammatory effects of the Mediterranean diet pattern. (You can check some of them out here and here) This diet emphasizes whole grains, fruits, and vegetables (with good amounts of olive oil and seafood), some dairy and poultry, and limited meats and sweets.
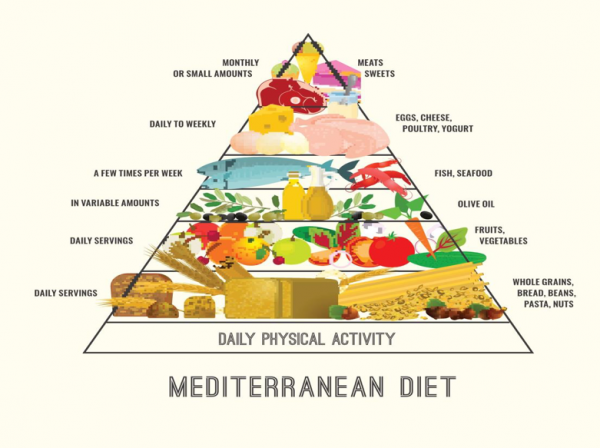 (Food pyramid courtesy of Oldways, oldwayspt.org)
(Food pyramid courtesy of Oldways, oldwayspt.org)
Spices have also been shown to have anti-inflammatory components and are a great way to flavor your foods. Tumeric, onions, garlic, ginger, and cinnamon all have been associated with lowering levels of inflammation, as have lignans (flax seed, whole grains, berries), olive oil, fiber, nuts, and magnesium.
Using your Newfound Knowledge
In summary, Charlotte says that it all comes down to this:
- Eat a diet high in omega-3 fatty acids and low in omega-6 fatty acids. Include cold water fish like salmon, mackerel, sardines, and herring)
- Eat a diet high in fruits, vegetables, and whole grains
- Limit simple carbohydrates
- Eat small meals
- Include leafy green vegetables, nuts, flax
- Avoid trans-fats
- Use spices when cooking
Inflammation and its impact on our health remains an important topic, so thank you to Charlotte and the UWMC for collaborating with us to share this information. The more we learn about topics such as inflammation, the better we can use food as a tool for our wellbeing. Let us know in the comments how you’re trying to fight inflammation with food, and what benefits you’ve noticed so far.
3 Thoughts on “Fighting Inflammation with Food”
On September 28, 2016 at 8:46 AM, Tonya said:
Reposting my comment from the Whole U eating well page: I see The Whole U is sponsoring a talk on the anti-inflammatory diet. Unfortunately it’s full, so I can’t register to attend. I am VERY curious at what’s going to be discussed there. At least it’s being given by a RD…but since there’s a lack of scientific evidence to support anti inflammatory diets, I wonder what exactly is going to be discussed and how. Links supporting my position: http://www.npr.org/2011/05/09/135844983/can-diets-fight-chronic-pain-the-science-isnt-there & http://www.arthritis.org/living-with-arthritis/arthritis-diet/anti-inflammatory/food-myths-arthritis.php .
So I ask….what peer reviewed information is available to support the claims of this session?
On September 28, 2016 at 11:32 AM, Jay said:
Very good, but you’ve conveniently left out that there’s an even more effective diet for combating inflammation and disease, and that is a fully vegetarian diet. Look up “blue zone diets”, the diets of people who live the longest. The Okinawa diet once consisted of mostly sweet potatoes, beans, and vegetables, with only 2% of calories from fish/meat/dairy/eggs, and those people regularly lived to age 100. The only people to have a longer average lifespan are the Seventh-day Adventist Vegetarians, who do not eat animal products at all. Omega-3s can be gotten from many plant foods, like nuts and seeds, especially flax seeds. Two tablespoons of ground flax seed a day in your cereal is enough. Add a B-12 supplement (since we no longer drink untreated water) and you’re set.
On September 28, 2016 at 3:53 PM, Charlotte said:
I definitely appreciate the comments and interest in this topic! The goal of this talk was to focus on overall dietary patterns shown to reduce markers of inflammation, one of the most studied being a Mediterranean style diet that is high in Omega 3 fatty acids from fish, nuts and high in fiber from legumes, fruits, vegetables and whole grains. Yes – definitely Flax seed is a great way to get more Omega 3s, Chia seeds are as well.
The site referenced in the first comment by Tonya has a good overview: http://www.arthritis.org/living-with-arthritis/arthritis-diet/best-foods-for-arthritis/
And for further reading here are some links to reviews and a recently published randomized controlled trial:
http://jn.nutrition.org/content/146/9/1684.long
http://content.onlinejacc.org/article.aspx?articleid=1137075
http://content.onlinejacc.org/article.aspx?articleid=1137818&resultClick=3
Comments are closed.